Every year over a million residents consult their GP with osteoarthritis. As implant designs and outcomes improve, more of these patients will receive partial or total joint replacements. Indeed over 75,000 knee replacements are done in England and Wales each year, making it the most common joint replacement. With better success rates in recent years, such surgery is being offered to progressively younger patients.
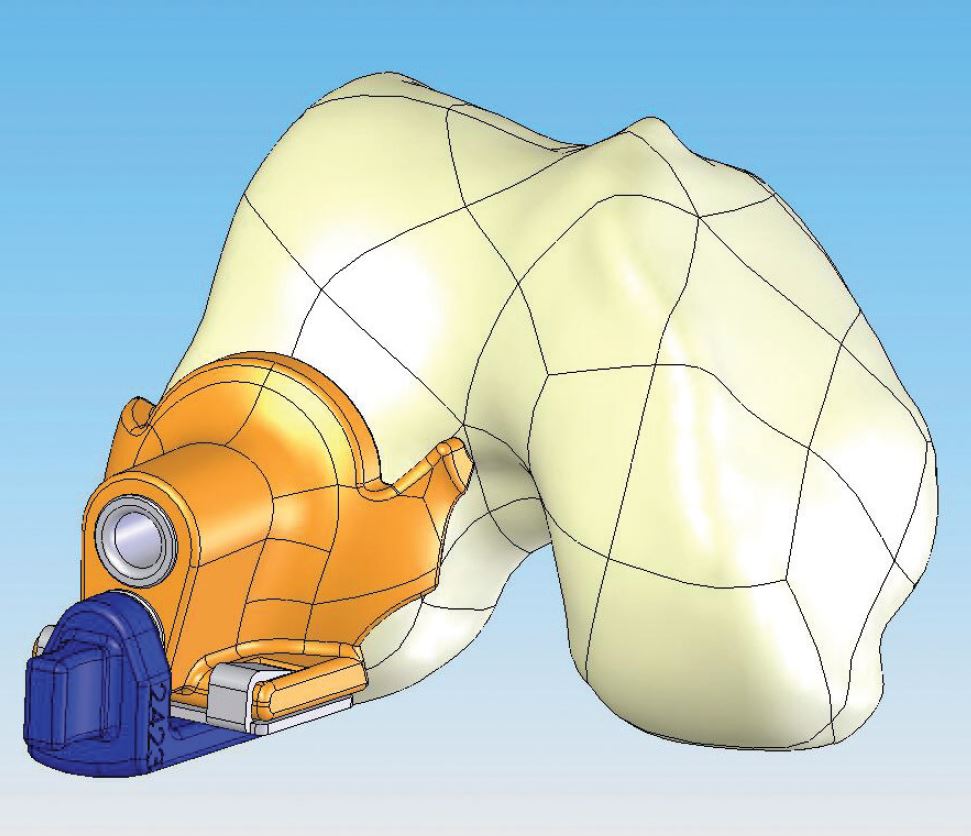
Custom Femoral Componant Custom Tibial Component Custom Femoral Cutting Jig
Problems with Conventional Designs
Increasing expectations of patients have led manufacturers to respond with continual improvements in design. However the range of sizes and shapes remains limited with conventional knee replacements and the surgeon still has to cut the bone to fit the implant using standard cutting jigs. This can result in under or over sized implants that do not conform to the patient's natural shape, causing an imperfect fit and a variable degree of precision in placing the implant.
Making the patient's bone fit the implant also requires more bone to be removed than may be really necessary.
New Developments
As a result of these limitations there have been a number of attempts to improve on conventional knee designs by the use of computer techniques and different groups have produced contrasting innovations. In 'computer-aided surgery', conventional knees are implanted to a higher degree of precision using computer navigation. 'Robotic surgery' takes this further by using a robotic device to make the bone cuts. Both add precision to the procedure, but neither utilizes a custom implant to maximize the value of this precise, data driven approach.
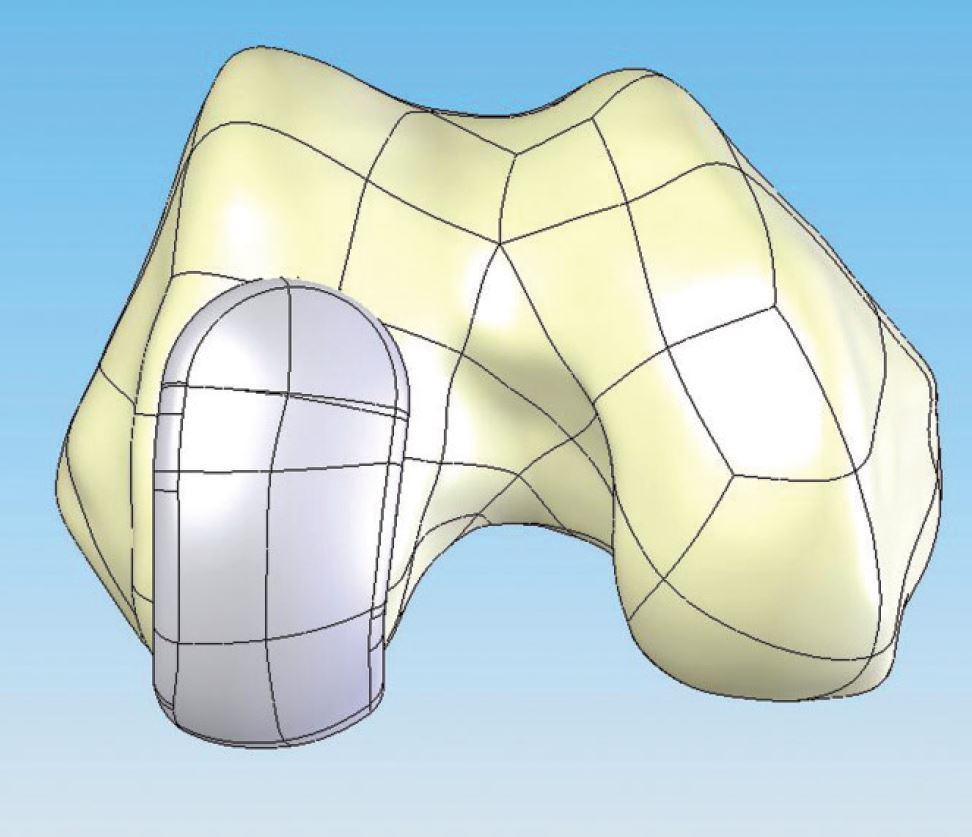
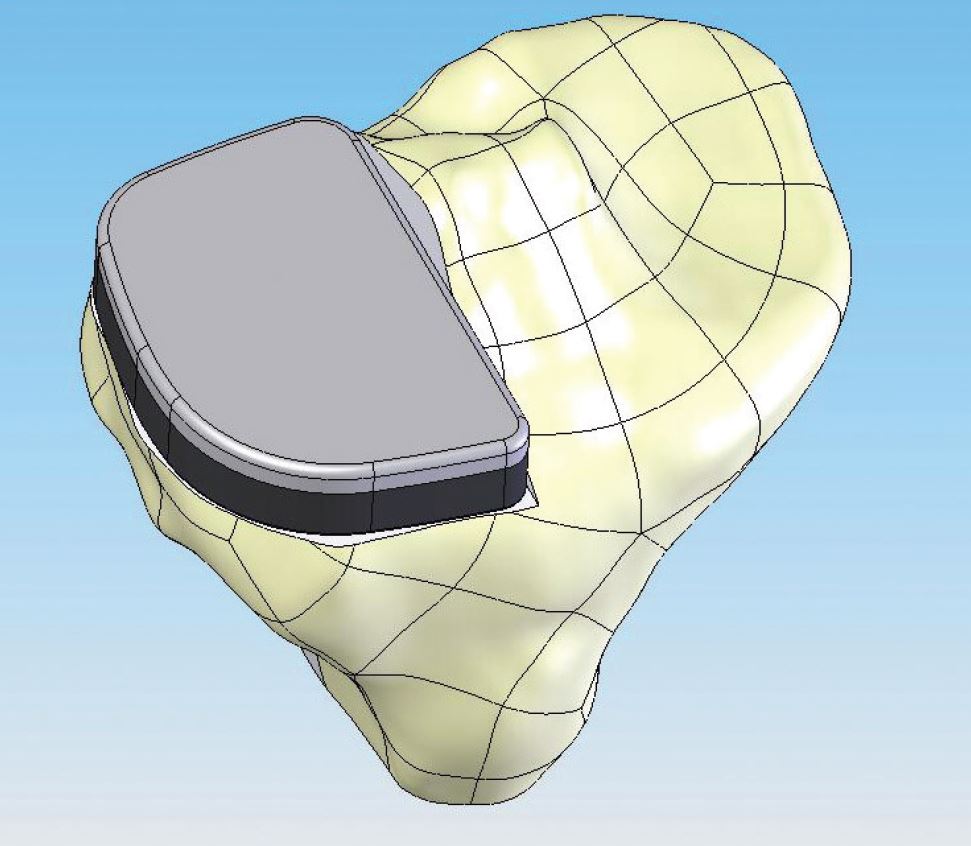
Recent advances include the ability to create custom implants using Computer Aided Design (CAD) software to convert CT and MRI scans into 3D models of the patient's knee. From these models, manufacturers create an implant made specifically for the patient. This enables the production of a knee implant that preserves cartilage and bone structure and custom instruments that address all types of osteoarthritis of the knee
This 'image-to-implant' technology is a significant improvement on existing computer-aided surgery and on conventional knee designs. Implants that correspond to the individual size and geometry of the patient enable the joint to be resurfaced rather than replaced, with less bone loss, less trauma and a simpler technique.
How a custom implant is created - a case study
Let's take the patient with medial compartment osteoarthritis (where the thigh bone meets the shin bone). The present trend is towards partial knee replacement (UKR) due to the good long-term survival, and better kinematics (mechanics) of UKR compared with total knees (TKR). UKRs are as effective as TKRs and have better functional outcomes at 15 years. So let's say we want to produce a custom made UKR. What is the procedure?
At consultation, standard criteria are used to decide the type of surgery, in this case medial UKR. The surgeon arranges a CT of the knee and partial scans of the hip and ankle. The imaging centre then transmits this data to the manufacturer.
Once the data is received, the software program reconstructs a virtual 3D image of the patient's knee. By reference to the hip and ankle data the knee model is then placed in correct spatial orientation and using CAD a virtual implant is created allowing for appropriate correction of leg alignment.
The patient's bone morphology (shape and substance of the bone) drives the implant geometry resulting in patient-specific femoral and tibial components, that is one to fit the end of the thigh bone and one to fit the top of the shin bone. The data then drives computerised machinery that produces patient specific components.
The same technology creates a custom set of surgical jigs exactly matched to the implant and the patient. This ensures that the bone cuts correspond precisely to the geometry of the implant, giving an exact match between the shape of the patient's bones, implant geometry and surgical instrumentation.
Who will benefit?
While there is a strong case for using this new technology, criteria for its use will need to be established. For the moment most patients will continue to be fitted with off-the-shelf implants, but those with unusual geometry, the very large or very small, and younger patients with a greater risk of later revision are poorly served by the standard.
In such patients the case to expand the use of knee replacements that fit precisely, rather than less well fitting off-the-shelf designs, is compelling. They offer precise reproduction of shape and size, and more conservative surgery, akin to resurfacing rather than replacement.
As this technology advances, we will need to develop the synergies between custom made implants and robotic techniques; that will be the next challenge.
For more information on custom made knees please see this leaflet - Custom Knees Leaflet
Copyright London Knee Clinic 2014