Definition
The literal meaning of tendonitis is inflammation of a tendon although the term is often used rather more broadly to refer to pain within a tendon either due to injury, inflammation, degeneration or a vascular problem. The more general term that applies to all of these conditions is tendinopathy.
The commonest tendons affected by tendonitis around the knee are the:
- Patellar tendon
- Quadriceps tendon
- Ilio-tibial band
Symptoms
Common symptoms include a localised burning pain over the affected area which is generally worse on exercise and there is often tenderness on direct compression of the tendon concerned.
Tendinosis refers to chronic tendinitis with long term damage to the tendon at a cellular level. The tendon is often thickened and scarred and contracture of the tendon can occur.
Treatment
Most patients with tendonitis respond to conservative treatments such as:
- Rest
- Change in exercise regime
- Non-steroidal anti-inflammatory tablets
On some occasions a splint is recommended and specialised exercises are frequently prescribed with the help of a Physiotherapist. Where other methods have failed a steroid injection close to but not directly into the tendon may be of value. However these should not be repeated as they carry a risk of tendon rupture.
For those cases where symptoms are acute or where previous attempts at non-surgical management have failed, surgery is an option.
Surgical Treatment
Surgical treatment is rarely necessary but may be used to:
- Change the forces acting on the tendon by a realignment
- Excise the worst affected part of the tendon
- Insert new material to supplement the tendon
- Remove a bony prominence or spur causing friction
- Decompress the tendon by removal of scarred tissue allowing new in-growth of blood vessels.
Patellar tendonitis
The commonest tendon affected is the patellar tendon, a large flat tendon joining the lower end of the patella to the upper part of the shin bone. All parts of the tendon can be involved but the upper end just at the junction with the patella is the commonest region affected. Although often called Jumper’s Knee it is most commonly seen in runners.
The usual symptoms experienced is pain at the front of the knee just below the patella often worse in weight bearing knee flexion activities such as going down stairs, or hills and on squatting. Sitting for long periods can also exacerbate it.
|
|
|
MRI scan showing patellar tendonitis. There is pale area is inflammed and swollen.
|
Diagnosis is usually made clinically and this is confirmed on MRI or ultrasound scanning particularly when invasive forms of treatment such as injection or operation are proposed. Other conditions can cause similar symptoms including abnormalities of the lower pole of the patella, and the underlying fat pad. It can also be mimicked by a medial plica attached to the synovial membrane adjacent to the lower pole of the patella.
Conservative treatment includes single leg eccentric decline squats under the supervision of a physiotherapist. However it is wise to be sure of the diagnosis before commencing this as articular damage at the lower pole of the patella will be made worse by this exercise.
|
|
|
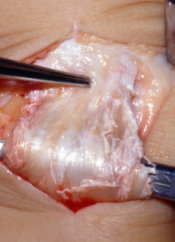
Operative view showing patellar tendonitis with degeneration of the tendon.
|
Recent pilot studies have suggested that platelet-rich plasma injections, can aid healing of the tendon but this is at a very early stage of investigation. Extracorporeal shock wave therapy has also been tried. This is a form of ultrasound that can selectively break down affected tissues and encourage healing and is worth considering if other methods of treatment have failed.
Persistent symptoms from patellar tendonitis that has failed to respond to other non-surgical measures might need surgical tendon decompression. This requires a small open surgical procedure in which an incision is made at the front of the knee and the central inflamed portion of the tendon is excised. At the same time, it is occasionally suitable to perform a knee arthroscopy if it is necessary to exclude other potential active pathology within the knee.
Surgical treatments include simple decompression, removal of bony spurs from the lower end of the patella and excision of the affected portion of the tendon and this can be done arthroscopically or by an open technique. Where patellar tendinitis occurs in the presence of patella alta distal transfer of the patellar tendon may be indicated. Rarely replacement of part of the tendon with a tendon graft may be required.
Quadriceps Tendonitis
This is generally a much less severe problem than patellar tendonitis and is less commonly encountered. It affects the lower end of the quadriceps tendon where it attaches to the upper pole of the patella. The pathology is similar to patellar tendonitis but the healing capacity of the quadriceps is much greater due to its greater blood supply and healing is generally faster.
Treatment is along similar lines to patellar tendonitis but surgery is rarely required.
Ilio-tibial Band Syndrome
A very common condition in runners, symptoms include pain over the outer side of the knee, usually coming on after exercise and very often only after a certain distance has been run.
The ilio-tibial band is a long strap like structure running the length of the thigh, crossing the knee on its outer side and attaching to the upper tibia at a small bony lump called Gerdy’s tubercle. During flexion and extension of the knee the lower end of the ITB moves backwards and forwards over the underlying lateral femoral condyle and its attached soft tissue structures. This constant movement between the tissues can set up an inflammation in the layers of tissue that glide over each other hence the concept of ‘ilio-tibial band friction syndrome’.
Tightness of the ITB can predispose to the condition. Local anatomical variants also contribute, such as bony swelling over the lateral femoral condyle. Leg alignment issues also contribute, for example running with the feet turned due to a torsional abnormality in the tibia can add extra strain on the ITB triggering the problems
Most treatment is conservative including:
- Rest
- Avoidance of activities that trigger symptoms
- Non-steroidal anti-inflammatory tablets
- Physiotherapy including stretching the ITB
- Local steroid injections
Surgery is very rarely performed and involves a small incision over the outer side of the distal thigh. Some of the fibres of the ITB are divided just above the area where the ITB crosses the lower femur and not directly at the site of pain. This takes the tension off the ITB resulting in resolution of pain in most cases. Following surgery running is generally resumed within about three months.
ITB Friction Syndrome Animation
TEXT Copyright London Knee Clinic 2014