Definition
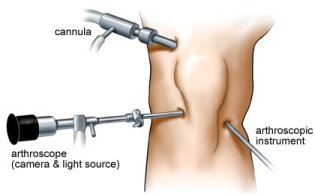
Arthroscopy means examination of the inside of a joint, such as the knee, using an instrument inserted into the joint through a small incision. Arthroscopy using instruments similar to those now used was first performed in the late 1960s. Over the years components of arthroscopes and the cameras to which are attached have steadily improved and now provide very high definition digital images. This enables them to be used for accurate diagnosis and surgical treatment of knee problems through tiny key-hole incisions.
What types of problem can be treated by arthroscopic surgery?
Many knee conditions are amenable to arthroscopic surgery and these are referred to elsewhere in this website under the heading of conditions. The following lists some of the common types of conditions that can be treated:
- Articular cartilage lesions such as chondral defects
- Fat pad lesions
- Ligament injuries such as anterior cruciate tears
- Loose bodies either bony or cartilaginous
- Meniscal tears
- Osteoarthritis
- Plica syndrome
How is an arthroscopy done?
In most cases we use a general anaesthetic. The reason for this is that in order to be able to move the knee freely and access all parts of the joint we need complete muscle relaxation. It is very difficult to achieve this under local anaesthesia. At least two small incisions are used and we call these arthroscopic portals. The incisions are usually between 4 and 8 mm in length. The position of the portals depends on what needs to be done and which part of the joint we need to reach.
|
|
In order to get a clear view the synovial fluid, normally a clear straw coloured liquid, is washed out of the knee which is continuously irrigated with very dilute saline using a pump. The pressure of the saline can be adjusted to provide the right amount of inflation and to enable blood and loose fragments to be washed out of the joint during surgery. Various sizes of arthroscope are available but typically a 4 mm diameter telescope is used in the knee introduced through a thin metal sheath. The arthroscope is attached to a fibreoptic light source and a camera enabling images to be displayed on a monitor so that the operating surgeon can see the interior of the knee. Various instruments can be inserted through the portals in the course of carrying out the surgery.
|
|
|
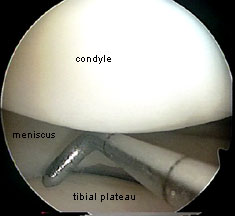
View at arthroscopy
The metal probe is 2 mm in diameter
|
What can be done during an arthroscopy?
A number of types of surgery can be performed. These include:
- Abrasion chondroplasty – shaving of rough areas
- Debridement of damaged tissues
- Excision of plicae and other synovial abnormalities
- Mechanical removal of damaged superficial layers of cartilage
- Microfracture of exposed bone to encourage healing
- Radiofrequency removal of abnormal tissues – radiofrequency ablation
- Reconstruction of ligaments such as the ACL
- Release of tight structures such as the lateral retinaculum
- Removal of damaged areas within the fat pad
- Removal of loose bodies
- Smoothing of rough articular surfaces
- Trimming or repair of meniscal lesions
What is the post-operative recovery like?
While you are still asleep, the knee is injected with a local anaesthetic and a synthetic lubricant so at the end of the procedure most people feel little pain. If significant pain does occur you need to let the nursing staff know and you will be supplied with pain killers in the recovery room and in the day case ward
Once you get back to the day case ward you will probably just want to sleep for a while. However most people are sufficiently awake for a light lunch following which the Physiotherapist will help you get out of bed and start walking. You will usually be up and about between 2 and 3 hours after returning from theatre. Once fully mobile you will be allowed home. Most people do not require sticks or crutches. However we prefer you to be accompanied rather than try to make your way home alone. Don’t forget you have had a general anaesthetic and surgery so it’s better to have someone with you.
If some cases more major surgery will have been performed and a slower more cautious period of mobilisation will be required. If crutches or a brace are prescribed it may take an additional couple of hours to get moving and in some cases you may need to stay overnight. It would be useful to ask about that before coming in for surgery so that you are prepared.
Generally patients coming from abroad who would otherwise be going out to a hotel room are offered an overnight stay so please ask about this before admission. Rarely complications occur that require you to stay overnight, the commonest being delayed recovery from anaesthesia. Persistent oozing from the arthroscopy portals can also rarely delay discharge.
TEXT Copyright London Knee Clinic 2014